Most discussions regarding airway management probably relate to use of airway devices during anaesthesia, in-hospital and out-of-hospital cardiac arrest (OHCA) and Emergency Medicine (EM). Each of these disciplines presents its own challenges, but perhaps the most hostile and challenging environment in which to manage the airway is during combat by those involved in Special Operations Medicine (SOM).
A report published in the Spring 2013 edition of the Journal of Special Operations, entitled, Proposed Change: Supraglottic Airways Committee on Tactical Combat Casualty Care (CoTCCC) Recommendation Paper, included a review of the use of Endotracheal Intubation (ETI) v Supraglottic Airways (SGA) and Surgical Airways v SGAs.
Many of the discussion points regarding use of ETI v SGAs will be familiar to most civilian practitioners of airway management and much of the evidence presented in the paper relates to non-military, non-combat situations. However, the paper does note that ETI ‘has been reported to be accomplished by military physicians on the battlefield with a success rate comparable to that achieved in the civilian setting.’ It also makes the point that intubating a trauma patient without sedation and paralysis will be difficult and that training courses that emphasise use of ETI and SGAs, often don’t discuss how to intubate or insert an SGA in a non-comatose patient.
Referencing a 2011 study by Timmerman, the paper also highlights that ‘SGAs may not be well tolerated by casualties who are not unconscious and may not be effective in casualties with direct airway trauma. The ideal casualty for SGA use is one who is unconscious and has no direct maxillofacial or neck trauma.’
The section discussing Surgical Airways v SGA is particularly interesting. Clearly, airway management in combat is not the same as management of a cardiac arrest patient in a civilian setting. The most common cause of airway death in combat casualties is maxillofacial trauma, with the result that management of the airway may be ‘complicated by blood, distorted anatomy, and a struggling patient.’
Referencing the manual by Butler et al, entitled, Prehopsital Trauma Life Support Manual (7th edition) – Military Version, published in 2010, the paper states that , ‘Many casualties with isolated maxillofacial injury can protect their own airways by simply sitting up, leaning forward, spitting out the blood in their airway and continuing to breathe in that position. Surgical airways should be reserved for those casualties in whom this strategy is not successful at maintaining an adequate airway. Maxillofacial injury should not trigger a knee-jerk reflex for the medic to attempt a surgical airway.’ Nonetheless, the TCCC noted that a surgical airway was the airway procedure of choice in a combat casualty when the airway is compromised by direct maxillofacial trauma.
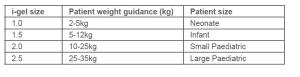
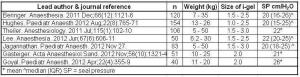
There is an interesting discussion regarding pre-hospital cricothyroidotomy and the records from the Joint Theater Trauma Registry, including the differences in failure rates for cricothyroidotomy between combat medics, physicians and physicians’ assistants and the caution that should be exhibited when interpreting this data. There is also a review of some of the published evidence regarding different types of SGA, including the Laryngeal Mask Airway, LMA ProSeal® , Combitube®, King LT and the i-gel. Inevitably, since this report was completed last year, additional evidence has been published regarding the civilian use of SGAs and ETI during cardiac arrest, which the committee may have wanted to include had it been available to them.
The conclusions of the report include the following:
- The recommendation for supraglottic airway use in Tactical Evacuation Care should be expanded to include SGAs other than the Laryngeal Mask Airway and Combitube®.
- Use of SGAs is recommended as both a combat medic and a combat paramedic skill.
- Casualties who are unconscious from haemorrhagic shock or severe Traumatic Brain Injury (TBI) but who have not suffered direct airway trauma are likely to be the best candidates for SGAs among the combat wounded.
- Casualties who are able to tolerate either ETI or SGA without sedation and paralysis are likely to have a poor prognosis.
Sadly, the latter refers to the point that the among the combat wounded, the most common causes of unconsciousness are haemorrhagic shock and severe TBI. Both associated with high mortality.
Clearly, there are many combat situations where management of the airway is best achieved by techniques other than insertion of an SGA. However, when use of an SGA is indicated or appropriate, it would seem sensible that the device should be one which can be reliably inserted quickly and easily, incorporates a gastric channel to reduce the risk of aspiration (compared to an SGA without a gastric channel) and has a high seal pressure. A 2nd generation SGA would therefore probably seem a more logical choice than a 1st generation SGA.
Whilst this paper concluded that the recommendation for supraglottic airway use in Tactical Evacuation Care should be expanded to include SGAs other than just the Laryngeal Mask Airway and Combitube®, it did not make any specific recommendation regarding use of 2nd generation devices. This may be an interesting area for the committee to consider in any future review.
The Journal of Special Operations Medicine web-site can be accessed at the following web address http://www.jsomonline.org